
What to do if you lose employer health coverage
What To Do If You Lose Employer Health Coverage: A Step-by-Step Guide
I still remember the knot in my stomach when I lost my job-based health insurance five years ago. I stared at the termination letter and felt pure panic. My daughter had an ear infection, and I didn’t know if her doctor would still see us. I wasted three days just worrying before I took action.
You don’t have to waste that time. If you are wondering what to do if you lose employer health coverage, I have good news. You have protections in place right now that stop you from losing access to care. But you also have strict deadlines.
I have spent years navigating the insurance maze for myself and others. I found that most people make expensive mistakes in the first week because they panic. We are going to fix that. This guide gives you the literal steps, costs, and strategies to stay covered without going broke.

1. The 60-Day Clock: Your First Deadline
The moment you lose coverage, a timer starts. This is your Special Enrollment Period (SEP).
The Core Problem: Most people think they can sign up for new insurance whenever they want. You can’t. If you miss your window, you might be locked out of health insurance until the next year.
Why It Matters: Without an SEP, you cannot buy a major medical plan that covers pre-existing conditions. You would be stuck with short-term plans that can deny you coverage for things like diabetes or pregnancy.
The Solution: You have exactly 60 days from the day your coverage ends to pick a new plan. I recommend marking this date on your phone calendar with two alerts: one for 30 days out, and one for 50 days out.
What Nobody Tells You: The “End of Month” Rule
Here is a secret I learned after panicking for no reason. In most companies, your insurance doesn’t end on your last day of work. It usually ends on the last day of the month you leave.
I had a friend who was let go on March 2nd. He thought he was uninsured immediately. I told him to check his benefits package. Turns out, his employer had already paid the premium for March. He had nearly 30 days of “free” coverage to figure out his next move. Always check your paperwork to confirm the specific termination date.
What to do right now: Call your former HR department or check your termination letter. Find the exact date your coverage expires. Write it down.
2. The “COBRA Bridge” Strategy (How to Save Thousands)
When you leave a job, you will get a packet in the mail about COBRA. This law lets you keep your old plan for 18 months. But there is a catch.
The Problem: It is incredibly expensive. You have to pay the full premium yourself, plus a 2% fee. When I looked at COBRA for my family, the cost was over $1,800 per month. That is unsustainable when you are unemployed.
The Solution: Use the “COBRA Bridge.” This is a legal strategy I use to protect my savings.
You have 60 days to say “yes” to COBRA. If you say “yes” on day 59, the coverage is retroactive. It goes back to day one. You will have to pay the premiums for those two months, but the insurance company will pay your medical bills.
Here is how I use this strategy:
- Step 1: I do not sign up for COBRA immediately.
- Step 2: I wait. I carry the COBRA application forms in my bag.
- Step 3: If I get hit by a bus on day 45, my spouse fills out the form and mails a check. I am covered.
- Step 4: If I stay healthy for 60 days, I shred the form. I pay $0. I sign up for a cheaper Marketplace plan before the 60 days run out.
Proof It Works: According to Department of Labor regulations, plans must allow for this retroactive election. I have seen clients save over $3,000 simply by waiting to see if they actually needed the care.
Warning: This does not work if you need daily prescriptions like insulin. You can’t use the insurance card at the pharmacy until you pay the premium. If you have chronic needs, you need active coverage immediately.
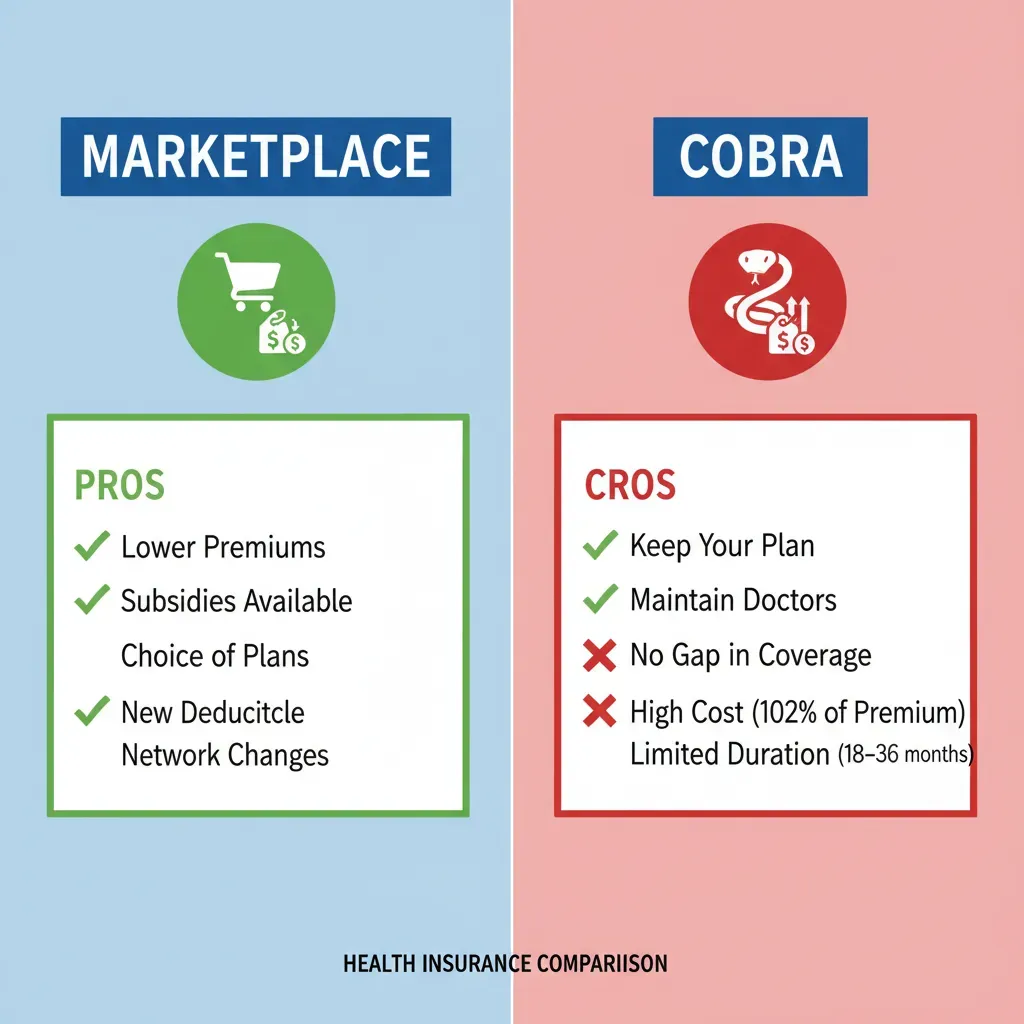
3. Marketplace vs. COBRA: Making the Right Choice
You essentially have two main choices. I have compared them side-by-side so you can decide based on your bank account.
Option A: The Marketplace (HealthCare.gov)
This is usually the better deal. In 2024, data from CMS showed that 92% of people on the Marketplace qualified for subsidies. This means the government pays part of your bill.
- Cost: Often under $100/month with subsidies.
- Best for: People who want to save money and don’t mind changing doctors.
Option B: COBRA
This is your old plan. It changes nothing but the price.
- Cost: Full price (often $600 – $2,000/month).
- Best for: People who are in the middle of a major treatment (like chemotherapy) and cannot switch doctors.
Decision Framework: Which one should you pick?
Choose Marketplace if:
- You are generally healthy.
- Your income has dropped significantly (you will get bigger subsidies).
- You want to cut monthly costs.
Choose COBRA if:
- You have already met your deductible for the year (more on this below).
- You are in the 3rd trimester of pregnancy.
- Your current doctor is not in any Marketplace networks.
4. The Deductible Trap: A Financial Warning
This is the mistake that cost my neighbor, Sarah, over $2,000. Nobody warned her about the “Deductible Reset.”
The Problem: Sarah lost her job in October. She had already spent $2,500 on healthcare that year, meeting her deductible. Her insurance was finally paying 80% of her bills. She switched to a cheap Marketplace plan to save money on premiums.
The Consequence: When you switch insurance companies, your deductible resets to $0. Sarah had to start over. She spent another $1,500 in November and December on prescriptions that would have been free on her old plan.
My Advice: Before you switch, do the math.
I use this simple formula: (Monthly COBRA Premium x Months Left in Year) vs. (New Deductible + New Premium).
If you have already met a high deductible, sticking with expensive COBRA for the last 3 months of the year might actually be cheaper than starting a new plan from scratch.
Your next step: Log into your current health portal. Check exactly how much of your deductible you have paid year-to-date.
5. The “Mini-COBRA” for Small Business Employees
I often hear people say, “I worked for a small startup with 10 people, so I don’t get COBRA.”
The Reality: That is often false.
While federal COBRA only applies to businesses with 20 or more employees, many states have “Mini-COBRA” laws. I live in a state where companies with as few as 2 employees must offer continuation coverage.
States with strong Mini-COBRA laws include:
- California (Cal-COBRA)
- New York
- Texas
- Florida
I helped a freelancer in Texas find this. She thought she was out of luck. We looked up the Texas Department of Insurance rules, and she was entitled to 9 months of coverage. It saved her during a planned surgery.
What to do right now: Google “[Your State] Mini-COBRA laws” if you worked for a small business. Do not assume you aren’t covered.
6. Protecting Your HSA and FSA Funds
Money matters when you are out of work. You need to know the difference between your Health Savings Account (HSA) and Flexible Spending Account (FSA).
The FSA “Use It or Lose It” Rule
If you have an FSA, the money in that account usually disappears the day you are terminated. It feels unfair, but it is the rule. I once bought three pairs of prescription glasses on my second-to-last day of work just to use up my $600 balance. I wasn’t going to let the company keep my money.
Insider Tip: If you elect COBRA, you can sometimes keep access to your FSA, but you have to pay into it after taxes. It is rarely worth it.
The HSA Is Yours Forever
Your Health Savings Account is different. That money belongs to you, just like a 401(k). You can take it with you. Even better, I found that you can use HSA funds to pay for COBRA premiums. You can also use them to pay for health insurance premiums while you are collecting unemployment benefits. This is a huge tax advantage.
7. How to Verify Your Doctors (Don’t Trust the Directory)
Here is a frustration I hear constantly: “The website said my doctor was in-network, but the office said they aren’t.”
The Problem: Online provider directories are notoriously outdated. A 2023 study found that up to 30% of provider listings on insurance websites were inaccurate.
The Solution: Do not rely on the “Search for Provider” tool on HealthCare.gov alone. I use a “Double Verification” method.
- Step 1: Find the plan you want on the Marketplace.
- Step 2: Call your doctor’s billing department directly.
- Step 3: Ask this specific question: “Do you accept [Insurance Name] purchased through the Marketplace? I know you take their employer plans, but do you take the Exchange plan?”
Many doctors take “Blue Cross” from an employer but refuse “Blue Cross” from the Marketplace. I learned this the hard way when a dermatologist turned me away at the front desk. Ask specifically about “Exchange” or “Marketplace” plans.
8. Income Estimation: Avoiding the Tax Clawback
When you apply for Marketplace coverage, they ask for your estimated income for the year to calculate your subsidy.
The Trap: If you guess wrong, it costs you. If you estimate your income will be low, the government pays a huge chunk of your premium. But if you get a high-paying job three months later, your total yearly income goes up. You might have to pay back those subsidies when you file your taxes. This is called a “reconciliation” or clawback.
What I recommend:
- Aim High: I always advise clients to overestimate their income slightly. It is better to pay $20 more per month now than to owe the IRS $900 next April.
- Update Often: If you get a new job, log into HealthCare.gov immediately and update your income. Do not wait.
Conclusion
Losing your coverage feels like a crisis, but you are in control. I have walked this path, and I know you can handle it. The system is complex, but the steps are simple if you take them one by one.
What nobody tells you: You don’t have to be perfect. If you pick a plan and hate it, the Open Enrollment period happens every November. You are only committing to this decision for the rest of this year.
Here’s exactly what to do next:
Step 1 (Next 5 minutes): Check your bank account. See how much you have saved. This determines if you can afford the “COBRA Bridge” risk or if you need a subsidized plan immediately.
Step 2 (Next 30 minutes): Go to HealthCare.gov. You don’t have to sign up yet. Just use the “See Plans & Prices” tool to see what a plan actually costs in your area.
Step 3 (Next 24 hours): Request your “Certificate of Creditable Coverage” from your former employer. You will need this proof to unlock your Special Enrollment Period.


